 With a few precautions you can avoid becoming a target of Lyme disease or contracting other tick-borne illnesses.
With a few precautions you can avoid becoming a target of Lyme disease or contracting other tick-borne illnesses.
by Marie Majarov
A new digital SLR camera, I was ready to learn! Spring 2005, images of creamy-white bloodroot and mayapples lit up my LCD screen. Learn I did, with an eye-opening experience from an unexpected source: the black-legged tick, Ixodes scapularis, an organism barely larger than the period that ends this sentence. I did not feel the bite. I did not see the tick. Lyme disease!
I was lucky. About three weeks after my wildflower expedition, I developed the unmistakable classic signs and symptoms of early disseminated Lyme disease: a huge bull’s-eye rash (erythema migrans) resembling a 6-inch red expanding dartboard on my side, strong flu-like symptoms, headache, joint pain, stiff neck, facial palsy, serious visual problems (Awful for a photographer!), and overwhelming fatigue. The diagnosis was clear and I began a four-week course of antibiotics, the recommended treatment of choice. My vision cleared and I gradually recovered. Many victims are less fortunate; an estimated 20 to 40 percent do not develop the bull’s-eye rash and/or have only mild initial flu-like symptoms that abate quickly without prompt treatment or diagnosis. Later chronic, major, and often debilitating problems problems can ensue from this multi-system infectious and inflammatory disease.
The poppy seed-sized blacklegged tick, also referred to as a deer tick, is a clever, teardrop-shaped parasite, and the vector or carrier for Lyme disease, the number one vector- born infection affecting humans in the United States and one of the fastest-growing infectious diseases in North America. The incidence of Lyme disease has increased dramatically over the past 20 years in Virginia. Medical complexities of this illness began unfolding in 1975 in Lyme, Connecticut. The first Virginia case was reported to the CDC in 1984. Now, 200 to 300 cases are reported annually from our Commonwealth. Since accurate data collection is problematic, this is likely to be a significant underestimate. Research is ongoing to find a safe vaccine for this endemic disease.
Prevention Par-tick-ulars!
- Wear light-colored, smooth, closely-woven clothing so ticks can be readily visible and have difficulty grabbing onto fabric.
- Wear a hat, long sleeves and pants; tuck your shirt into your pants and pants into socks. Tall, non-laced boots without eyelets are recommended.
- Masking tape can be used to seal junctions between socks and pants, and at the waist for extended work or hunting in tick-infested areas.
- Permethrin on clothing, sprayed according to manufacturer directions, is the single most important “par-tick-ular” prevention according to Profs. Rob and Ann Simpson. They credit their freedom from Lyme, through many years exploring and documenting the wilds of Virginia, to regularly spraying: pants, socks, shirts, hats, coats, and underwear! Spray must be totally dry before clothes are donned.
- DEET products properly sprayed on exposed skin can be useful, but don’t rely on these alone!
- Frequently inspect for ticks on yourself, your children, and your pets during outdoor activities and especially after undressing. Groin, navel, armpits, waist, head and behind knees and ears are especially vulnerable. Remember, black-legged ticks are teeny and easily missed; a magnifying glass can be helpful.
- When coming in from the field, dry outdoor clothes at least 20-30 minutes in the dryer to kill any ticks attached to them.
- Avoid tall grass and dense vegetation; stay on cleared paths and trails whenever possible.
- Don’t encourage deer to feed in your yard. Clear brush and leaf litter from around your home and yard; keep lawns mown.
- Talk to your veterinarian about tick protection products for your pets; pets can bring ticks into your yard and/or home.
- Hunters need to keep themselves protected when cleaning carcasses; wear rubber gloves.
- If you have been in tick-infested areas and experience illness or rash, it is imperative to tell your physician about your tick exposure!
This article originally appeared in the May 2006 issue of Virginia Wildlife magazine. You can download the article, in its original formatting and photography, as a PDF file. If you enjoyed this article, consider subscribing to Virginia Wildlife for more stories and insight on the natural world, supplied by the state’s leading wildlife and outdoor experts!
Dr. David Gaines, State Public Health Entomologist at the Virginia Department of Health (VDH), states that black-legged ticks and Lyme infection have steadily become more common in Virginia counties along the Potomac River, Chesapeake Bay, and Atlantic Ocean. Wider, ongoing, up-to-date infection surveillance and tick testing are being strongly encouraged by VDH throughout Virginia. These villainous ticks are a year-round menace, but the peak tick season is April through September.
The black-legged tick, however, is just a player in this emerging illness. The causative factor in Lyme disease is actually a corkscrew-shaped bacterium, Borrelia burgdorferi (Bb), lurking in the tick’s midgut. Possessing unique and confounding abilities to change shape and cloak themselves within the human immune system, these bacteria can hide effectively, seriously complicating early detection and decisions about treatment.

Other prominent characters in this tale of ticks and disease include our endearing white-tailed deer and more than 30 host species of small mammals, birds and reptiles. The big stars are white-footed mice that serve as especially competent reservoir hosts, places where Bb live harmlessly and reproduce. The tiny acorn nourishes this entire troupe of hosts. A legion of 99 different bird species accepts hitchhiking ticks.
Deciduous forests, nearby grassy areas (including lawns & picnic areas), and brushy, shrubby transitional zones called “edge habitat” are all favored romping grounds for this infamous black-legged tick. Female ticks lay masses of 2,000 eggs in rich, moist, protective leaf-litter in early spring. Larva, nymph and adult stages follow in the tick’s two-year life cycle with one blood-feast being enjoyed in each stage. By summer, eggs hatch into larvae, slurping their first meal, blood, often Bb rich from juicy-eared white-footed mice. Satisfied, larvae molt into nymphs that become dormant until the next spring when, as the air warms, they awaken very active and hungry!
Eighty-percent of all bites to humans comes from this ravenous pinhead-sized nymph. Mine did. Famished nymphs do not jump, run, fly, or leap; they simply climb to the top of a blade of grass or bit of leaf-litter and transfer themselves to any host (even an unsuspecting nature-photographer) that brushes by their waiting place. The nymph “quests” upward for blood. It secretes an anesthetic to make its bite painless and a chemical to keep the host’s blood from clotting and inflammation nonexistent, all so its presence will go unnoticed. A cement-like substance enables attachment long enough (24-48 hours) for it to suck all the sustenance it needs for the coming year. Bb bacteria may be in an infected nymph’s saliva or regurgitated up through the intestinal tract into the straw-like mouthparts where they are easily passed to a host.
A final molt occurs as fall weather arrives. The new adult waits for another passer-by, perhaps a migrating bird that becomes an unknowing source of dispersal for this vector with its infected cargo. Whitetail deer are the preferred final host, providing ticks a warm and comfortable venue to spend their second winter, sup a final blood-feast, mate, drop to the ground, lay eggs and die.
Hikers, hunters, birdwatchers, bikers, fishermen, picnickers, gardeners, pets and children can all become inadvertent hosts for infected ticks. Dr. Richard Goode, a Northern Virginia veterinarian and avid turkey hunter, describes seriously elevated although all do not show clinical symptoms. The incidence of Lyme infection in our domesticated pets is a portent of the major health risk of Bb to humans. Dr. Goode feels spring is the most dangerous time for outdoor enthusiasts because of nymph activity. “No season is safe” Dr. Goode adds; he finds active ticks on turkey carcasses during warm winter days.
Two additional tick vector species are common in Virginia: the lone star tick, Amblyomma americanum, and the brown dog tick, Dermacentor variabilis. In Virginia, their associated diseases, Ehrlichiosis and Rocky Mountain spotted fever, occur with less frequency than Lyme disease. At this time, there is no conclusive evidence that either of these ticks are carriers carriers of Lyme bacteria. Dr. Gaines reports that the lone star tick is “the most commonly encountered tick in Virginia” and is suspected of carrying a less severe “Lyme-like disease” that is “probably self-limiting.” He further notes that our devious black-legged perpetrator can frequently carry multiple infectious agents.
Ticks have existed for 400 million years, and have a decidedly nasty reputation. However, in the larger ecological picture, ticks have been part of nature’s efforts to maintain overall ecological health, what Lord Fairfax Community College Professor of Natural Resources, Rob Simpson, calls the “constant competition and dynamic change in nature.” Dr. Gaines also wisely points out that today ticks help to “keep wild places wild” by discouraging most humans from freely roaming in, and often disturbing the delicate ecological balance of our natural treasures.
Ecologists Dr. Richard Ostfeld and Dr. Clive Jones of the Institute of Ecosystem Studies in Millbrook, NY, using the Mountain Lake Biological Station here in Virginia as one of their study-sites, looked closely at the web of ecological connections among hosts, habitat, disease and oak mast-acorns. They found that when acorn crops are highest, mice and deer populations explode; soon after, the number of ticks and incidence of Lyme infection also soar. These are valuable insights toward the prediction and awareness of disease patterns. Further, their work points to the importance of biodiversity and our impact in this regard. Extinction of predators (ex. mountain lions and wolves), eastern agriculture moving westward, reforestation, and fragmentation of our forests as homes and development increasingly encroach on/into wooded areas have all contributed to huge increases in the number of deer and mice in now wooded urban areas.
My eye-opening lessons from Lyme disease were not just medical but also ecological. I developed an appreciation for the natural history of the black-legged tick and the remarkable ecological connections that are critical to understanding Lyme disease and effecting prevention and safety in our beautiful Virginia woods. Forest canopy ecologist and Virginia native Dr. Bruce Rinker says it eloquently, “Living in wooded regions means living responsibly: knowing the symptoms, understanding the treatments and preventions, acknowledging the ecological roles of vectors and pathogens, educating others, and supporting medical research.” Living in tune with nature.
Tick Removal
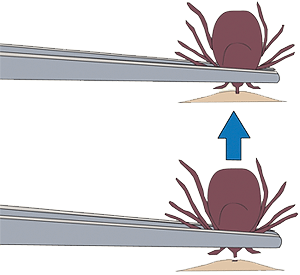
Remove a tick from your skin as soon as you notice it. Use fine-tipped tweezers to firmly grasp the tick very close to your skin. With a steady motion, pull the tick’s body away from your skin. Then clean your skin with soap and warm water. Throw the dead tick away with your household trash.
Avoid crushing the tick’s body. Do not be alarmed if the tick’s mouthparts remain in the skin. Once the mouthparts are removed from the rest of the tick, it can no longer transmit the Lyme disease bacteria. If you accidentally crush the tick, clean your skin with soap and warm water or alcohol.
Don’t use petroleum jelly, a hot match, nail polish, or other products to remove a tick.
Image courtesy of CDC, Division of Viral and Rickettsial Diseases.
For More Information
- Everything You Need to Know About Lyme Disease and Other Tick-Borne Disorders, second edition, by Karen Vanderhoof-Forschner, with forward by Dr. Willy Burgdorfer, © 2003.
- Lyme Disease, by Len Yannielli, © 2004.
- “Peril in the Understory,” Audubon Magazine, July 1999, 101: 74-82.
- Excellent educational materials, information, and pamphlets are available from the Lyme Disease Foundation and the Virginia Department of Health.
- Special appreciation is expressed to the many professionals who provided information and time to help with this article.

